Pre-transplant anti-porcine antibodies do not predict xenograft survival in pig-to-non-human primate orthotopic heart transplantation
Javier Galindo1, Avneesh K Singh1, Andy A Tully1, Alena Hershfeld1, Billeta Lewis1, Tianshu Zhang1, Bartley Griffith1, Muhammad M Mohiuddin1.
1Surgery, University of Maryland, Baltimore, MD, United States
Background: There is an increasing need to accurately screen candidates who may benefit from xenotransplantation. To date, the field has relied on flow-cytometric techniques using porcine cells to screen for anti-porcine antibodies (APA) in the sera of non-human primate (NHP) recipients. We sought to evaluate whether pre-transplant APA are predictive of recipient survival in our experience with pig-to-non-human primate (NHP) orthotopic heart transplants (OHTs). To do this, we performed a retrospective survival analysis incorporating pre-operative APA levels.
Methods: Fifty pig-to-NHP OHTs were performed from 2017 to 2024 at the University of Maryland, Baltimore. Pre-transplant recipient serum samples were assayed for anti-porcine IgG and IgM. Briefly, recipient serum was inactivated and incubated with porcine aortic endothelial cells (PAECs) of either donor origin or from an immortalized GGTA1 KO PAEC line.Binding was assessed by flow cytometry (Cytek Aurora or BD Accuri C6 Plus, CA) and analyzed using FlowJo software (FlowJo LLC, Ashland, OR). Normalized geometric mean fluorescence intensity (MFI) for the antibodies binding to cells was calculated and normalized to values obtained from serum from a baboon with confirmed rejection. Subjects with known or suspected perioperative cardiac xenograft dysfunction (PCXD, n = 24), were excluded from the analysis. Retrospective multivariate Cox proportional hazard regression analyses were performed using Stata/BE 18.0.
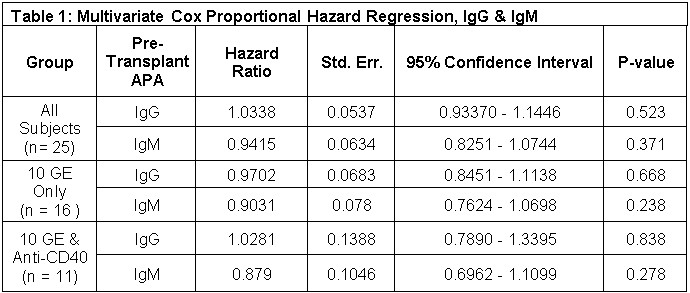
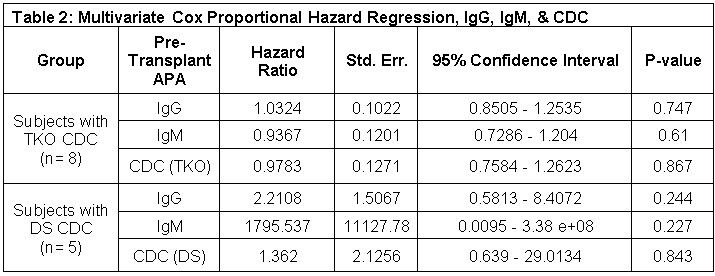
Results: Of 50 pig-to-NHP OHTs performed, 24 experienced PCXD and were excluded. Results of a multivariate Cox regression are shown in Table 1 and 2. Table 1 reports hazard ratios using all subjects for whom pre-transplant APA was available (n = 25), for 10 gene-edited (10GE) xenograft recipients only (n= 16) and for 10GE recipients receiving anti-CD40 (n = 11). In all cases, hazard ratios for pre-transplant IgG and IgM are not statistically significant with effects approaching 1 in all cases. A subgroup analysis was performed using subjects for whom pre-transplant complement-dependent cytotoxicity (CDC) was available using either triple-KO cells (GGTA1 KO, β4GalNT2 KO, CMAH KO, n = 8) or donor specific (DS, n = 5) PAECs (Table 2). Again, all hazard ratios are not statistically significant.
Conclusion: Our experience with pig-to-NHP OHT shows that pre-transplant APA are not predictive of post-transplant survival. In a more limited set of subjects, we find that pre-transplant CDC is also not predictive of survival. These results are unexpected and run counter to established practice in xenotransplantation. Possible explanations include the inherent variability of this technique as well as the possibility that overall APA measures obscure measurement of specific immunodominant APA. This result highlights the need to establish robust, standardized approaches to screening potential xenograft recipients.
[1] Cardiac
[2] screening
[3] antibody
[4] non-human primate