A survival analysis of pig-to-non-human primate orthotopic heart transplants
Javier Galindo1, Andy A Tully1, Avneesh K Singh1, Billeta Lewis1, Tianshu Zhang1, Alena Hershfeld1, Bartley Griffith1, Muhammad M Mohiuddin1.
1Surgery, University of Maryland, Baltimore, MD, United States
Background: Progress in this xenotransplantation has centered around progressive genetic modifications in donor pigs and the use of novel immunosuppressive agents. Despite the significant progress that has been achieved, there has not yet been a rigorous analysis of the survival benefit of genetic modifications or specific immunosuppressive agents. We performed a retrospective survival analysis to determine the relative survival benefit of specific genetic modifications and immunosuppressive agents.
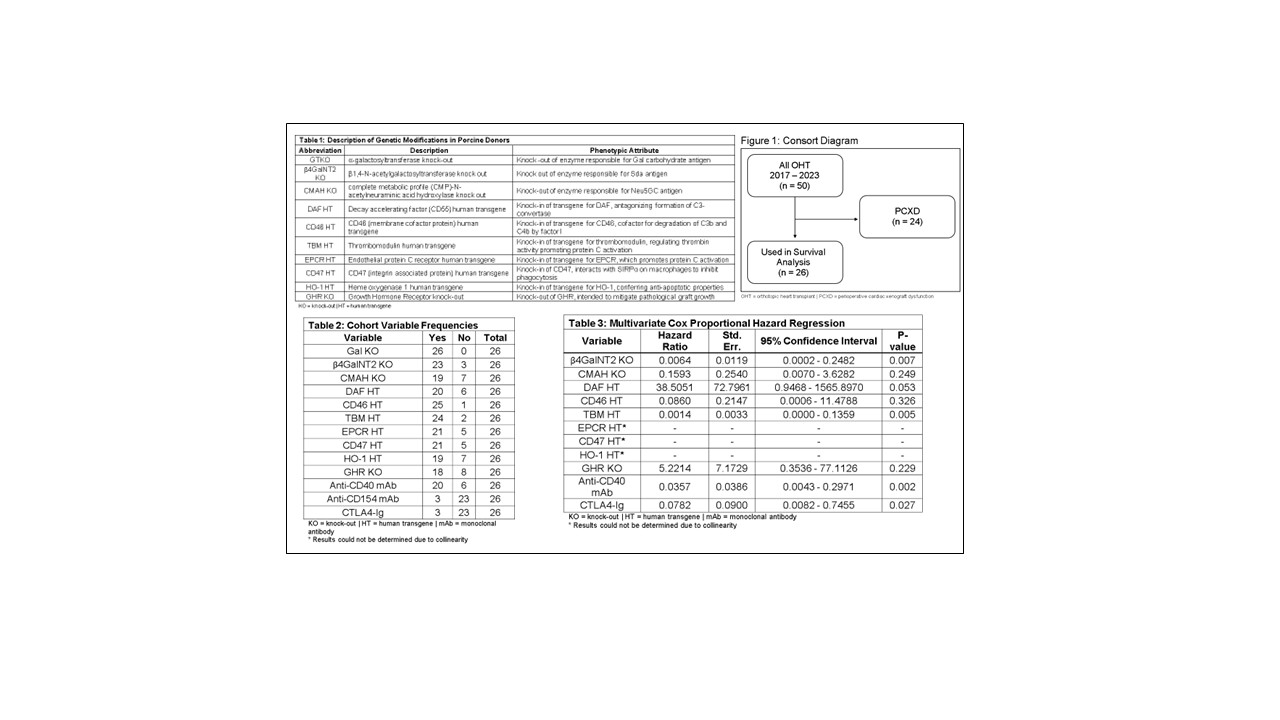
Methods: Fifty pig-to-non-human primate orthotopic heart transplants were performed between 2017 and 2023 at the University of Maryland, Baltimore. Porcine donors (Table 1) were obtained from Revivicor, Inc (Blacksburg, VA, USA). All subjects received induction immunosuppression with anti-thymocyte globulin, rituximab, glucocorticoids, and costimulation blockade (anti-CD40 mAb, anti-CD154 mAb, or Belatacept). Subjects with known or suspected perioperative cardiac xenograft dysfunction (PCXD, n = 24) were excluded from the analysis (see Figure 1). Retrospective multivariate Cox proportional hazard regression analyses were performed using Stata/BE 18.0.
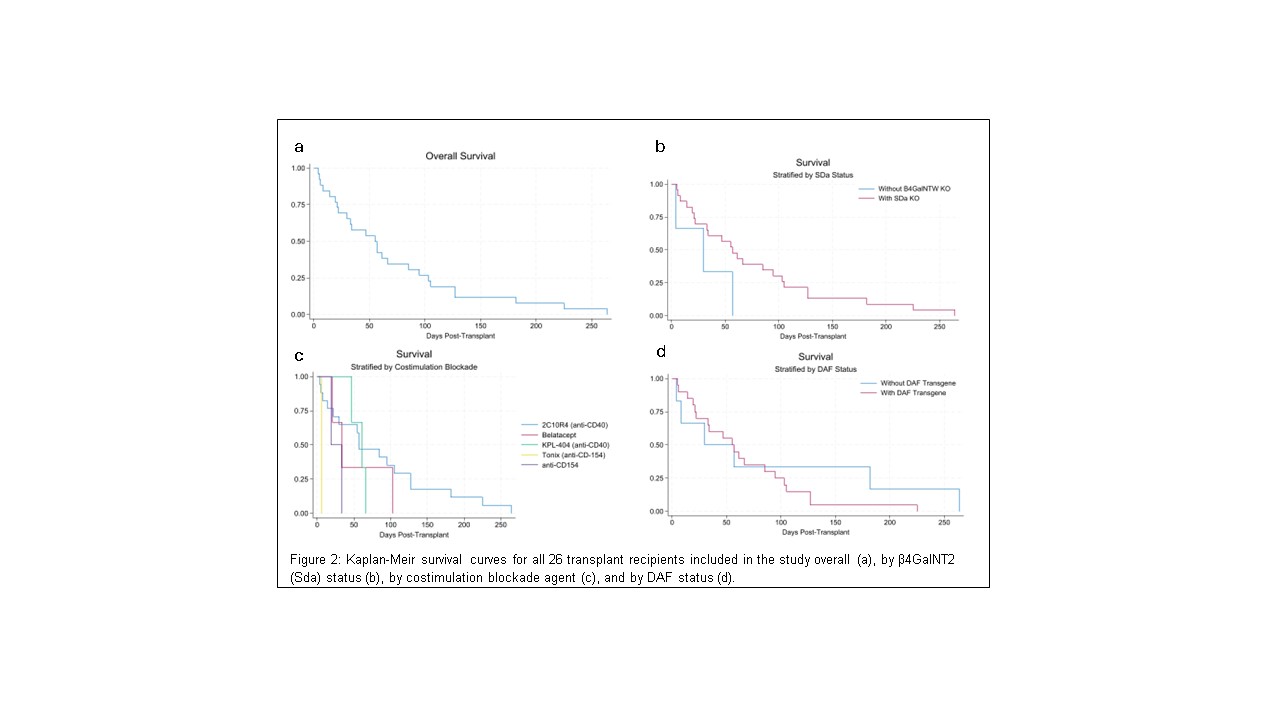
Results: A total of 50 pig-to-NHP OHTs were performed, of which 24 experienced PCXD and were excluded from further analysis. Among the remaining 26 subjects, survival ranged from 4 to 264 days with a median of 56 days (Figure 2a). Table 2 shows frequencies of variables for this cohort. Results of a multivariate Cox regression are shown in Table 3. β4GalNT2 KO and TBM HT showed a statistically significant survival benefit (HR 0.0064 and 0.0014, respectively). Anti-CD40 mAb and CTLA4-Ig showed statistically significant survival benefits (HR 0.0357 and 0.0782, respectively) as compared to use of anti-CD154 mAb. Curiously, inclusion of DAF HT showed a statistically significant survival penalty (HR 38.5051). This appears to be driven by two long-lived recipients of DAF HT negative xenografts (Figure 2d). Results for EPCR, CD47, and HO-1 could not be calculated due to collinearity.
Conclusion: This represents the first survival analysis informing the potential harm or benefit of specific genetic modifications or immunosuppressive agents in the xenotransplantation literature. While our results are limited by an ultimately small sample size, we are able to conclude that knockout of β4GalNT2 and inclusion of TBM HT conveyed a statistically significant survival benefit, while use of anti-CD154 mAb in the immunosuppressive regimen was associated with a statistically significant survival penalty. Inclusion of DAF HT appears to convey a large survival penalty although this effect may be driven by outliers and merits further investigation. Incorporation of data from additional prior studies (e.g., kidney transplants, heterotopic heart transplants) may add further statistical significance to enrich these results.
[1] Cardiac
[2] Heart
[3] orthotopic
[4] non-human primate