Assessment of allosensitization following pig-to-human xenotransplantation
Imad Aljabban1, Sue A Tiongko1, Jacqueline Kim1, Ian Jaffe1, Karen Khalil1, Tal Eitan1, Simon Williams1, Brendan Keating1, Aprajita Mattoo1, Vasishta Tatapudi1, Edward Skolnik1, Jeffrey M Stern1, Adam Griesemer1, Robert A Montgomery1, Massimo Mangiola1.
1NYU Langone Transplant Institute, New York, NY, United States
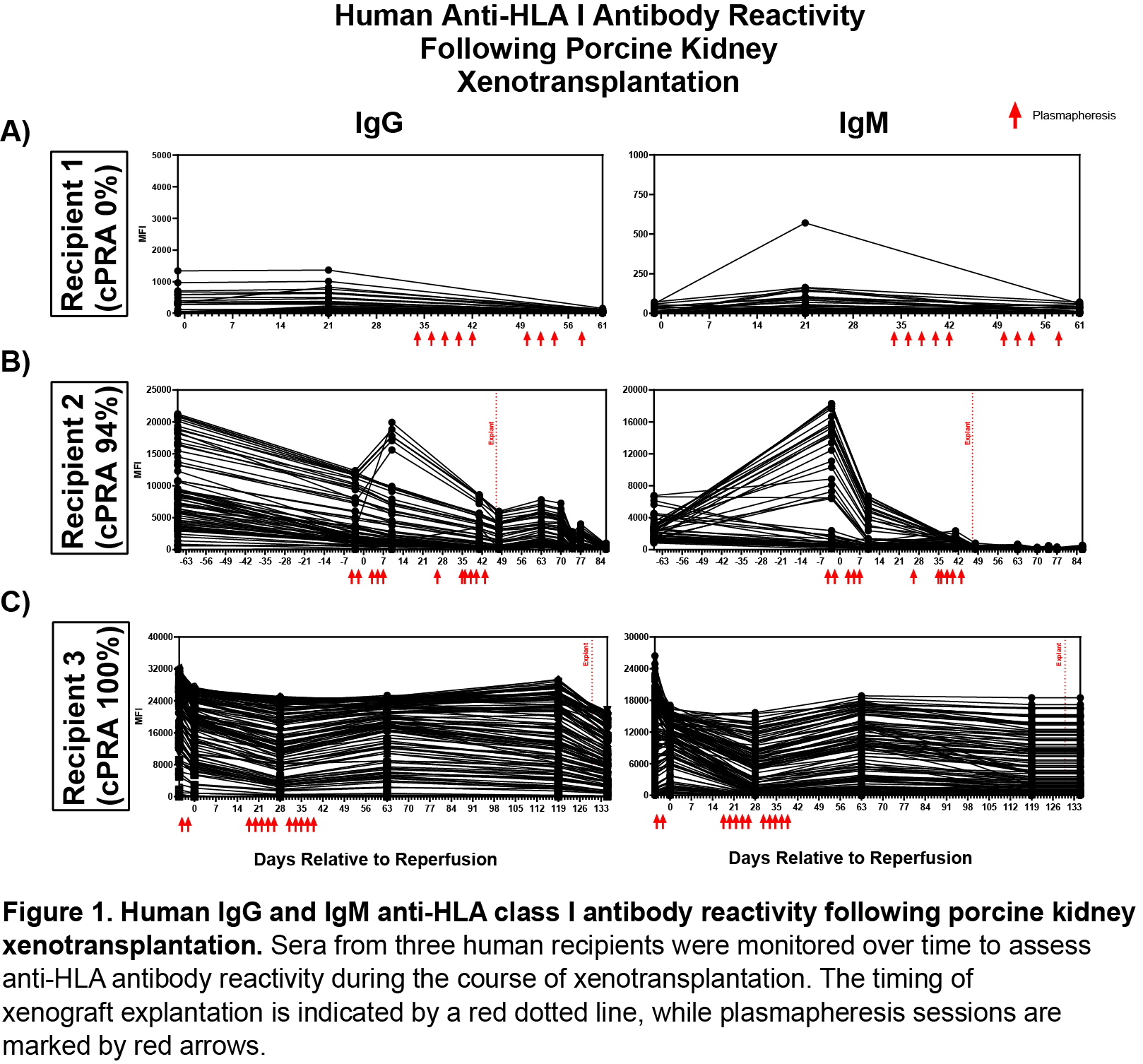
Introduction: Xenotransplantation presents a promising approach to addressing the organ shortage problem and has been proposed as a bridge to allotransplantation for patients at high risk of mortality while on the transplant waitlist. Concerns remain that exposure to pig antigens could increase alloantibody levels, potentially complicating future allotransplant eligibility. In this study, we examine anti-HLA class I and II response in three pig-to-human kidney xenotransplant recipients with varying degrees of pre-existing allosensitization to assess changes in alloreactivity post-xenotransplant.
Methods: Three pig-to-human kidney xenotransplants were performed at NYU Langone Health from 2023–2024 using clinically approved immunosuppression. Serum was collected from recipients at serial timepoints and tested for antibodies against human leukocyte antigen (HLA) class I and II antigens using a Luminex-based single antigen bead assay. Reactivity to HLA was quantified by determining the mean fluorescence intensity (MFI). To calculate the panel reactive antibody (cPRA), beads with an MFI ≥1000 were used. cPRA was calculated with the OPTN cPRA calculator.
Results: Recipient 1 was a brain-dead human decedent with a cPRA of 0%, who had previously undergone bilateral nephrectomy followed by implantation of a GGTA1 KO Thymokidney. The recipient was maintained for a planned duration of 61 days. Throughout the study period, both IgG and IgM anti-HLA Class I antibody reactivity remained consistently below the threshold for positivity (Figure 1A). Recipient 2 was a living human with a cPRA of 94% who underwent GGTA1 KO Thymokidney transplantation. By day 10, an increase in reactivity against HLA-B44, B45, and B82 was observed. However, 37 days following xenograft explantation, anti-HLA Class I reactivity across all specificities declined to levels well below pre-transplant values (Figure 1B). Recipient 3, also a living human, had a cPRA of 100% and received a 10 GE Xenokidney transplant. Anti-HLA class I antibody levels remained stable throughout the duration of xenograft implantation. The xenograft was explanted on POD 130, after which anti-HLA class I MFI values fell below baseline pre-transplant levels (Figure 1C). Across all three cases, IgM reactivity was less than IgG and anti-HLA Class II antibody reactivity remained negative (data not shown).
Conclusion: Although limited by follow-up duration, these data demonstrate no increase in anti-HLA class I and II reactivity following xenograft explantation.
Work funded in part by Lung Biotechnology, a wholly owned subsidiary of United Therapeutics Corporation..
[1] Xenotransplantation
[2] Human Leukocyte Antigen
[3] Allosensitization
[4] Kidney