Tao Li, People's Republic of China
Director of department
The department of kidney transplantation
The Second Affiliated Hospital of Hainan Medical University
Brain-dead human subjects as preclinical models for xenotransfusion: Feasibility and safety of genetically engineered pig red blood cell transfusion
Tao Li1, Hidetaka Hara1, Hongtao Jiang1, Huiling Gan1, Ting Yan1, Jianan Zhang1, Liang Xu1, Meng Yang1, Yong Wang2, Hang Yu1, Dengke Pan2, Yi Wang1.
1The Transplantation Institute of the Second Affiliated Hospital, Hainan Medical University, Haikou, People's Republic of China; 2Chengdu Clonorgan Biotechnology Co., Ltd, Chengdu, People's Republic of China
Objective: Xenotransfusion using genetically engineered (GE) pig red blood cells (pRBCs) offers a potential solution to blood shortages, particularly in emergencies. This study aimed to evaluate the suitability of brain-dead human subjects as a preclinical model for xenotransfusion by comparing their hematological and immunological profiles with those of acute blood loss (ABL) patients and assessing the feasibility, safety, and immunological responses to GE pRBCs in a brain-dead human subject.
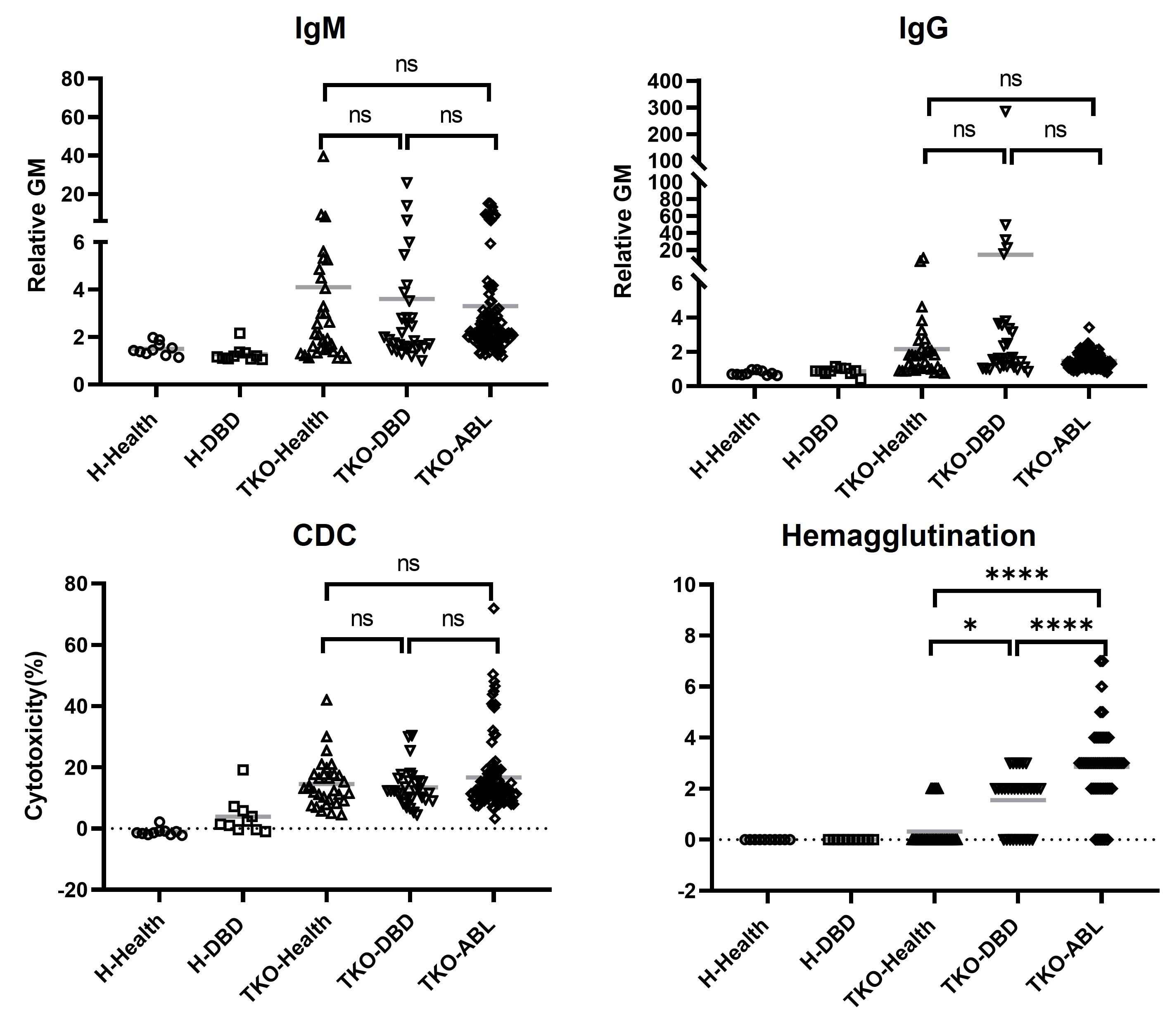
Methods: Comprehensive evaluations were conducted on hematological, biochemical, electrolyte, coagulation, and inflammatory markers, arterial blood gas parameters, and immunological profiles in brain-dead subjects (n=179) and ABL patients (n=104) requiring transfusion. In vitro assessments of anti-triple-knockout (TKO; lacking Gal, Neu5Gc, and Sda antigens) pig RBC responses were also performed in brain-dead subjects (n=31) and compared to those of ABL patients (n=102).
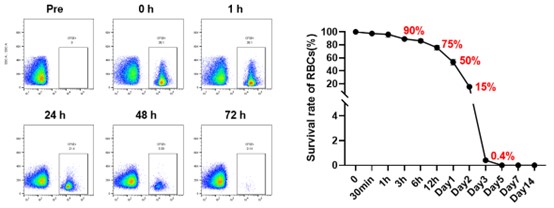
RBCs from TKO pigs expressing human CD55 (housed under pathogen-free conditions) were labeled with CFSE for tracking. A single brain-dead human subject received a transfusion of GE pRBCs, with pre-transfusion treatments including an anti-C5 inhibitor, corticosteroids, and antihistamines. Monitoring included continuous vital sign tracking, hematological and immunological assessments, complement activation assays, and pathogen screening.
Results: Comparative analysis revealed similar pathophysiological and immunological profiles between DBD and ABL patients, supporting the former’s relevance as a xenotransfusion model.
GE pRBCs exhibited survival rates of 50% at 24 hours, 15% at 48 hours, and were cleared by 72 hours. Pre-transfusion anti-pig IgM levels were low, transiently decreased post-transfusion, and rebounded by day 3. Anti-pig IgG levels, initially undetectable, significantly increased by day 7, accompanied by heightened complement-dependent cytotoxicity and hemagglutination. Both classical and alternative complement pathways were activated but moderated by regulatory mechanisms. No pig-derived pathogens were detected.
Conclusion: Brain-dead human subjects closely replicate the clinical conditions of ABL, providing a valuable preclinical model for xenotransfusion research, particularly in settings where nonhuman primate models have limitations. This study establishes the feasibility and safety of GE pRBC xenotransfusion, offering critical insights into immune responses and pathogen safety. The absence of zoonotic transmission and the manageable immune profile observed in this first-in-human trial underscore the potential of xenotransfusion as a promising solution to global blood shortages in critical care.
This study was supported in part by the National Key Research and Development Program (2023YFC3404304: Y.W., 2024YFC3406800: H.J.), National Natural Science Foundation of China (82260154: Y.W., 82460153: H.J., 82400891: T.L.) and Hainan Provincial Science and Technology Talent Innovation Project (Category B) (KJRC2023B08: Y.W.). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
References:
[1] genetically engineered pig
[2] brain-dead human subjects
[3] acute blood loss patients
[4] xenotransfusion
Lectures by Tao Li
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-02 15:05 - 15:55 |
Pre- and Subclinical Models 1 | Brain-dead human subjects as preclinical models for xenotransfusion: Feasibility and safety of genetically engineered pig red blood cell transfusion | Auditorium |
