Michael J. Friedlander Professor of Medicine
Medicine
Columbia University
Evidence for human thymopoiesis in a porcine thymus graft and T cell tolerance to the source pig in a living human recipient of a porcine thymokidney xenotransplant
Farshid Fathi1, Pinar Gur Cetinkaya1, Yasmeen S Saad1, Benjamin Vermette1, Jeffrey Stern2, Karen Khalil2, Jacqueline Kim2, Ian Jaffe2, Imad Aljabban2, Lars Burdorf3, Adam D Griesemer2, Robert A Montgomery2, Megan Sykes1,4,5.
1Columbia Center for Translational Immunology, Department of Medicine, Columbia University Medical Center, New York, NY, United States; 22Department of Surgery, Transplant Institute, New York University Langone Health, New York, NY, United States; 3United Therapeutics Corporation, Research Triangle Park, New York, NY, United States; 4Department of Surgery, Columbia University Medical Center, , New York, NY, United States; 5Department of Microbiology and Immunology, Columbia University Medical Center, New York, NY, United States
Study’s purpose: Porcine thymic transplantation tolerizes xenogeneic recipients to the porcine source animal in animal models. A 54-year-old woman with complex comorbidities received a composite thymokidney transplant from an GGTA1 knockout pig, achieving initial renal function before xenograft failure for non-immunological reasons on postoperative day (POD) 47.
Methods: Serial peripheral blood mononuclear cell (PBMC) samples were analyzed by spectral FCM, and mixed lymphocyte reactions (MLRs) were performed on purified T cells to assess tolerance. Thymocytes were isolated from the thymic portion of the xenograft explant and analyzed using spectral FCM.
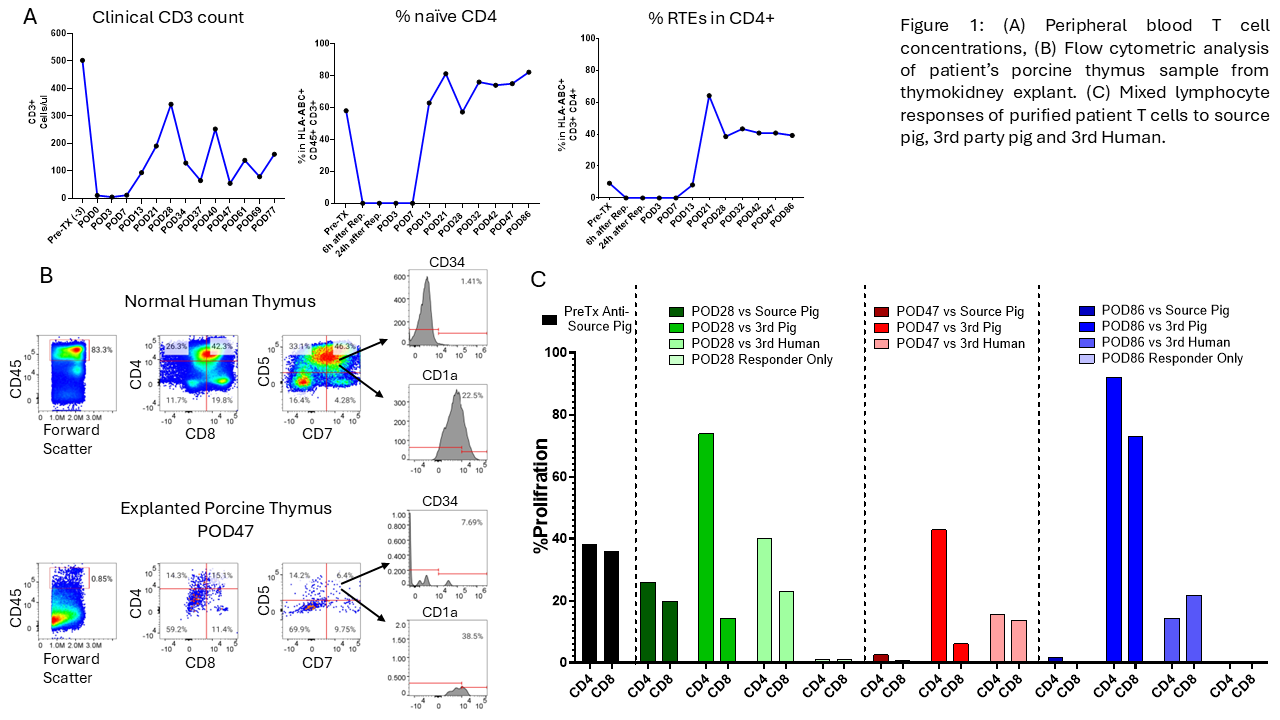
Results: T cell levels in peripheral blood declined to 10/µL post-induction therapy and recovered to a peak of 342/µL by POD28. By POD21, 64% of the recovering CD4 T cells displayed a CD45RA+CCR7+ "naïve" phenotype and expressed CD31, consistent with recent thymic emigrants (RTEs). Pre-transplant CD4 T cells included <10% RTEs (Figure 1A). FCM analysis on cells from the POD47 thymic xenograft revealed human CD45+ leukocytes (0.85%), including double-positive (CD4+CD8+), single-positive, and double-negative thymocytes. The double-negative cells expressed markers such as CD5, CD7, CD1a, and CD34, consistent with human T cell progenitors in the porcine thymus (Figure 1B). MLR results demonstrated progressive hyporesponsiveness toward the source pig with preserved responses to third-party pig and allogeneic human cells, achieving full donor-specific unresponsiveness by POD47 and POD86 (Figure 1C).
Conclusion: These findings suggest that a porcine thymus in a thymokidney xenograft supported human thymopoiesis and the development of T cells tolerant to the pig. Thymic transplantation is a promising approach to achieving T cell tolerance in xenotransplant recipients.
Lectures by Megan Sykes
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-02 17:10 - 18:45 |
Mentoring the future: A session to inspire young investigators | Xenotransplantation - five decades of progress | Auditorium |
|
Thu-02 08:30 - 10:00 |
Towards clinical xenotransplantation: Clinical trials are underway today! | Moderator | Auditorium |
|
Wed-01 15:05 - 15:55 |
Immunosuppression and Tolerance 1 | Evidence for human thymopoiesis in a porcine thymus graft and T cell tolerance to the source pig in a living human recipient of a porcine thymokidney xenotransplant | Auditorium |
|
Fri-03 12:00 - 13:00 |
Closing Plenary | Pig to human thymokidney transplantation | Auditorium |
